Looking Forward: How to End Pediatric AIDS in Our Lifetime
You are here
We see a future where pediatric AIDS does not exist.
This is how it happens.
It Starts with a Family
Elizabeth Glaser contracted HIV in a blood transfusion in 1981 while giving birth to her daughter, Ariel. Elizabeth had unknowingly passed the virus on to Ariel through breast milk and her son, Jake, had contracted the virus in utero. The Glasers discovered the only drugs on the market were for adults; nothing had been tested or approved for children. Ariel lost her battle with AIDS in 1988. Fearing that Jake’s life was also in danger, Elizabeth rose to action.
She approached her close friends for help in creating a foundation that would raise money for pediatric HIV/AIDS research and later change the course of history for families impacted by HIV around the world. Elizabeth lost her own battle with AIDS in 1994, and to honor her legacy, the Pediatric AIDS Foundation was renamed the Elizabeth Glaser Pediatric AIDS Foundation (EGPAF).
To Families Around the World
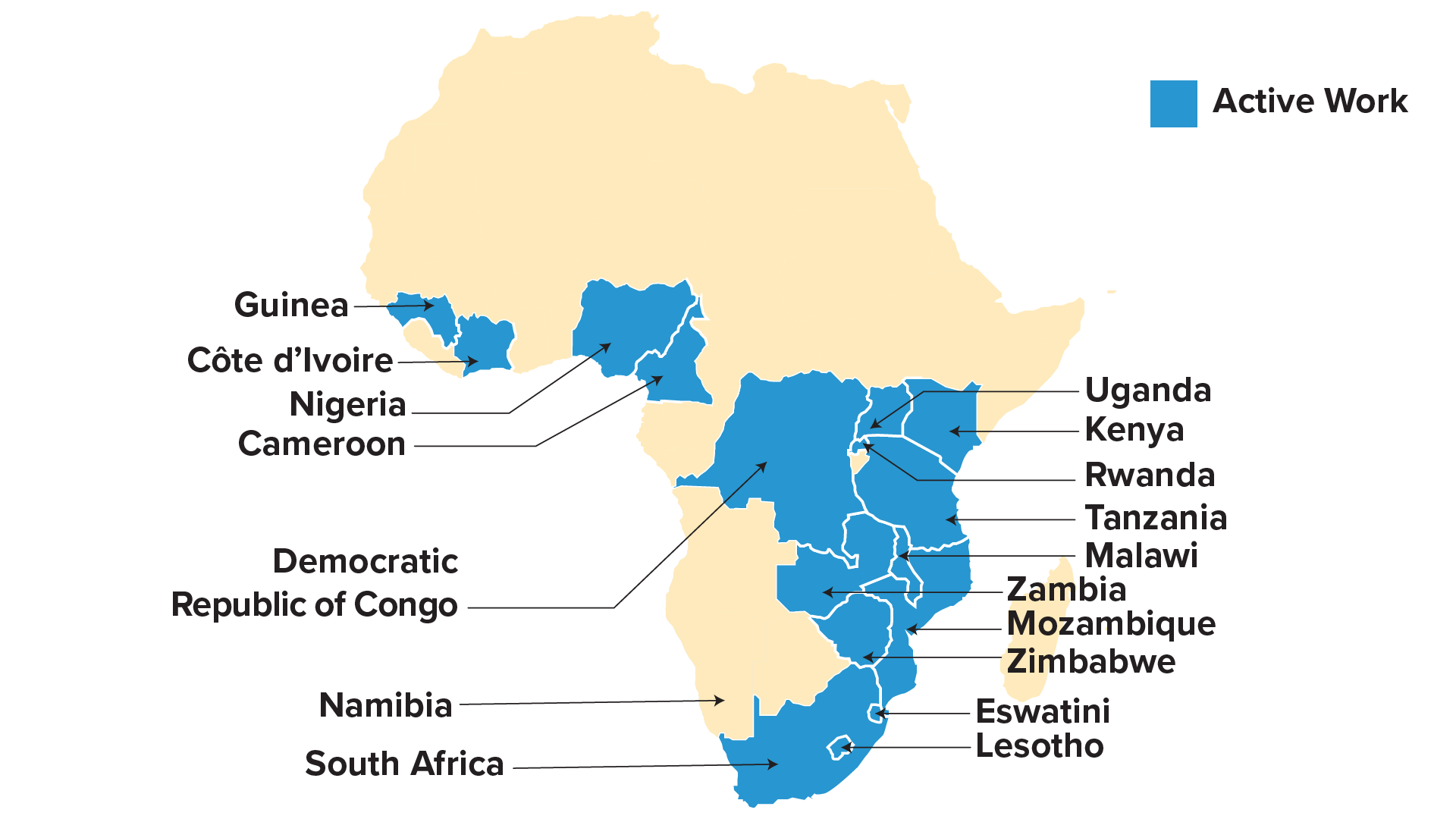
In 1999, EGPAF launched one of the first global programs to bring antiretroviral therapy to pregnant women to prevent HIV transmission to newborns. The foundation rapidly scaled up following the creation of the President’s Emergency Plan for AIDS Relief (PEPFAR) by George W. Bush. More than two decades later, EGPAF currently works in 17 countries and has reached over 34 million pregnant women with services to prevent transmission of HIV.
Where Are We Now?
Despite Amazing Progress, the Global AIDS Response is Failing Children
The number of children acquiring HIV has dropped by over 60% since 2010 – a tremendous accomplishment in the fight against HIV. And yet, children who are living with HIV are less likely to know their status, less likely to be on treatment, and less likely to be virally suppressed than adults. These growing inequities result in children bearing a disproportionate share of AIDS-related deaths.
Too many families are still losing far too many children, even when the tools exist today to save these children’s lives.

Progress Towards the Elimination of Vertical Transmission (EVT)
In 2023, roughly 300 children acquired HIV each day. Almost all these cases could have been prevented. Transmission can occur from mother to infant in pregnancy, during childbirth, and through breastfeeding. However, the risk of vertical transmission drops to less than 2% if a mother is on antiretroviral therapy (ART) and remains virally suppressed for the duration of the pregnancy and postpartum period.
Progress towards eliminating vertical transmission has been uneven – with wide variations across geographical regions.
How to Close the Gaps for Mothers
Providing prevention and treatment for pregnant women is one of the great successes of the HIV response. However, this progress has not budged for the last ten years.
One size does not fit all mothers. These tools to close the gaps in maternal care should be tailored to a particular context and consider each client’s specific needs.

Expand Primary Prevention
The best way to keep an infant HIV-free is to prevent the mother from ever becoming HIV-positive.
All women should have access to comprehensive prevention services – including PrEP and other new prevention technologies– before, during, and after pregnancy.
Learn how mothers in Nigeria are getting the support they need.
Increase ART Coverage
The percentage of pregnant women on ART has not meaningfully increased in over a decade.
Linking all women with lifelong treatment is critical for the health of mother and baby.
Learn how a mother in Lesotho is sticking with treatment for her son.
Ensure Retention Through Breastfeeding Period
Preventing vertical transmission doesn’t end at birth.
Treatment adherence and ongoing retention in care can decrease the substantial portion of new infections that occur during breastfeeding.
Learn how a mother in Eswatini prevented transmission thanks to partner support.Read Nurse Maya’s story and learn how she has watched Eswatini be transformed in the past 20 years.
Children Need Care: Pediatric Treatment
Antiretroviral therapy is lifesaving for children living with HIV. If not on treatment, 50% will die by their second birthday and 80% by the age of five. Despite this, pediatric treatment rates have fallen significantly behind adults. Pediatric coverage is 20 percentage points lower than adult coverage.
2023 marks the largest disparity between children and adult treatment coverage in the history of the HIV epidemic. Children are the age group least likely to receive treatment. This is not just a lag in outcomes, but a persistent, unconscionable inequity.
Finding the Missing Children
One-third of children still do not know their HIV status. Testing is the first step towards ensuring children with HIV are linked to treatment. These strategies can help.

Point-of-care early infant diagnosis
POC diagnostics speed up the time from when an HIV-exposed infant is tested and when their caregiver receives the result. This allows faster initiation of ART for HIV-positive children, therefore reducing severe illness and death.

Index testing
60% of children living with HIV who are not on treatment are over the age of 5, and therefore won’t be reached through early diagnosis. Testing all children of people living with HIV is a key tactic for finding older children with HIV who have not yet learned their status.
Learn how Nigeria is closing the testing gaps to ensure more children living with HIV get the treatment they need.
Optimizing Treatment
When children have access to the treatment they need, they are able to thrive. Optimizing pediatric treatment starts here.

Reduce Drug Development Delays
It takes years before new drugs approved for adults are available for children, often resulting in sub-standard pediatric care. Clear regulatory guidance and innovative trial design combined with incentives for drug developers can help to shrink these time delays.

Develop Child-friendly Formulations
Pediatric antiretrovirals are often bitter, hard for children to swallow, and difficult for caregivers to correctly dose. The recent rollout of pediatric dolutegravir has the potential to improve treatment outcomes.
Additional palatable fixed-dose formulations that are easy to crush, chew, or sprinkle into food help ensure children living with HIV are getting the medications they need.
Learn how children like Sheldon are gaining access to the essential medicine they need.
Viral Suppression
The ultimate goal of HIV care is to ensure clients can live a long, healthy life, regardless of HIV status. When a child living with HIV is virally suppressed, he or she is less at risk of other opportunistic infections, like tuberculosis, advanced HIV disease, or ultimately, death from HIV-related causes. Viral suppression is also a key prevention strategy, as people living with HIV with an undetectable viral load cannot transmit to others.
And yet, children continue to face lower rates of viral load testing and significantly lower rates of viral suppression than adults.

Improving Adherence
It’s not enough for children to start treatment, they must stay on treatment to remain healthy. Patient and caregiver education, psychosocial support, and differentiated service delivery – like dispensing multiple months of medication at once or having a special day for children to come to a health facility – can help.
Learn how a young man in Nigeria is supporting other adolescents.
Expanding Viral Load Testing
HIV viral load testing is a critical tool for antiretroviral treatment (ART) monitoring and optimization and can serve as a necessary signal for the need for a patient to transition to a better regimen. Viral load data also can be used to improve programming, therefore improving viral suppression.
Learn how community workers are supporting viral load testing in DRC.
Ensuring Social Protection and Quality of Life
HIV status is only one facet of a person’s life. Advancing quality of life through access to education, nutrition support, gender equity, comprehensive health care, and child protection is essential to ensure mothers and children can thrive.
Learn how a young woman from Malawi is helping others build a better life.
Preventing Mortality
A lack of access to optimized treatment puts children at an increased risk of death. In 2023, children accounted for only 3% of all people living with HIV but comprised 12% of all AIDS-related deaths. Improving antenatal and pediatric care can decrease preventable deaths from all causes – not just HIV.
Learn how a loving caregiver can be a game changer for a child living with HIV.Where Do We Go From Here?
It is Possible to End Pediatric AIDS
The Elizabeth Glaser Pediatric AIDS Foundation has been deeply committed to ending AIDS in children for over 35 years. And we will remain steadfast in this promise until the job is done, until an AIDS-free generation is achieved.
In the words of Elizabeth Glaser herself, “Sometimes in life there is that moment when it’s possible to make a change for the better. This is one of those moments.” Join us in fighting for these changes.

*Many of the children whose faces are shown in these photos are HIV-free.



