Ismail Harerimana, 32, was a community health worker in Kabale, Uganda, when funding for his position was paused and then terminated in 2025. Seventy health workers with HIV expertise were let go at the hospital where he worked.
“We’re all supported through donor programs. And when the Stop Work order came, contracts were ended. Clinics closed, and those remaining are overstretched,” he reports.
Since that time, Ismail has been continuing his work the best he can without a salary. He tries to track the children and women who were receiving HIV care at the hospital where he worked, many of whom live in villages far from the facility. Compounding this difficulty is the reality that many patient records were not maintained when HIV staff was let go.
“Everything was disorganized. People died. We have had so many young people get lost [from the system],” he says. “Just like that.”
Ismail reports that “Uganda’s HIV response is still standing, but it’s weaker and fragile.” Basic HIV services have resumed at health centers: drugs are available and HIV testing has resumed. But that is not enough, says Ismail. At his location on the southwestern edge of Uganda, community systems are as vital as clinical services. “Who is checking on the health of people who do not show up at the facility?” he asks.

“Adherence counseling, stigma reduction, and youth engagement are treated as optional, so they’re not being really supported,” says Ismail, “yet they have a long term and essential outcomes.”
“When mothers miss appointments or lose access to follow-up care, it means that the mother is in danger of passing HIV to her child” and both become vulnerable to illness and death. Peer groups, counseling, and other psychosocial programs help families seek treatment. Without those interactions, prevention of mother-to-child transmission has become more fragile, Ismail says.
“I’m just praying so hard [that community programs resume] because what has been happening is really, really so bad.”
Ismail has lived with HIV his entire life, having acquired it from his mother during pregnancy, childbirth, or breastfeeding. It is only because of the arrival of PEPFAR funding and programs that he survived childhood. Beyond the medicine, a peer support group was a lifeline for him and kept him on treatment. This experience drives Ismail’s passion to reach vulnerable children, even without a salary.
Just before Christmas, an administrator at the hospital where Ismail volunteers reached out to him, asking him to take on an official position again as a community health worker. It is still unclear if he will be paid, but he sees this as a step forward after a difficult year.
“I know that I have a task to bring back children. It might be hard to get them back, but it is my mission.”
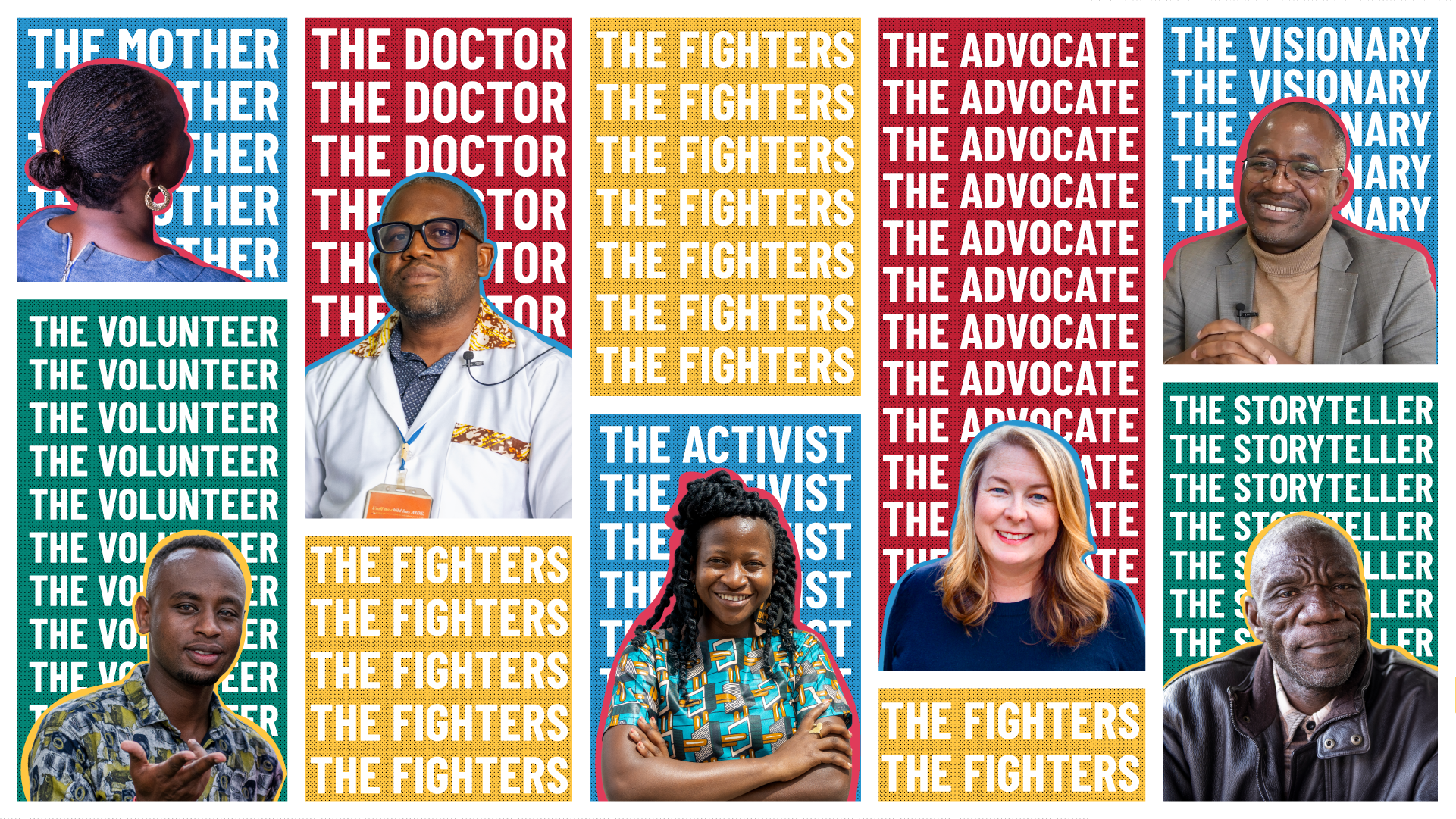
Ismail Harerimana