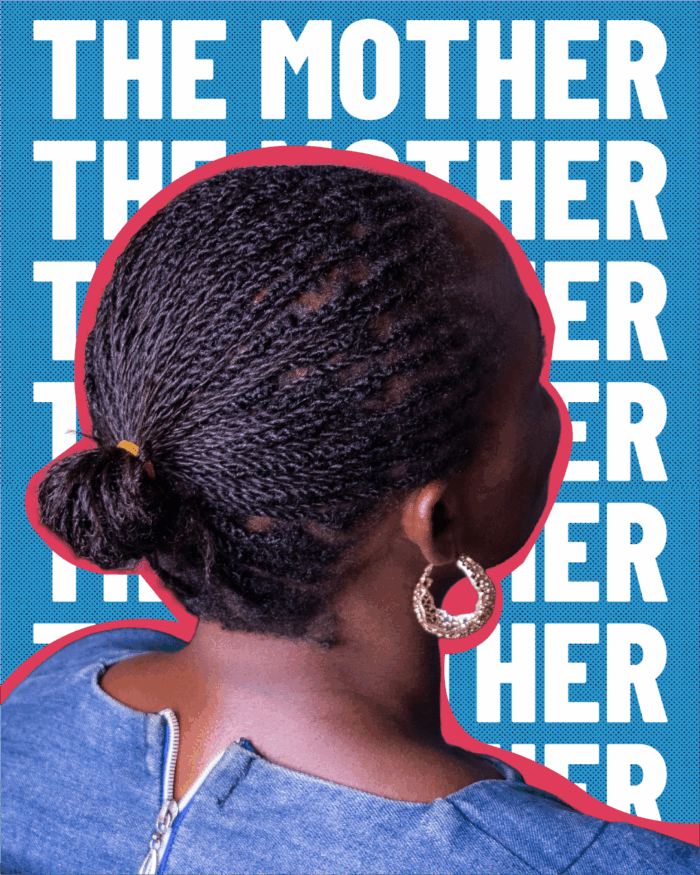
“Children need protection, care, and hope for the future,” says Mary*, a mentor mother living in southwest Uganda with three children, one girl and two boys.
The mentor mother program was established by nongovernmental organizations in collaboration with the Uganda Ministry of Health under the United States President’s Emergency Plan for AIDS Relief (PEPFAR). The program trained mothers living with HIV to counsel other women about the importance of adhering to treatment throughout pregnancy and breastfeeding so that their children can grow up HIV-free.
Mary has been on both sides of the mentor mother relationship, at one time receiving advice from a mentor and then becoming a mentor herself. Two of Mary’s children are HIV-free thanks to her own adherence to prevention of mother-to-child HIV transmission services.
When the Stop Work order was issued last year, the mentor mother program was halted. Beyond that, Mary and many others in her community became alarmed that lifesaving antiretroviral (ARV) medication would not be available.
“My son and I completely lost hope. We believed our lives would end soon and that there was no future for us.”
“The fear and stress were so heavy that we almost took our own lives. That period left deep emotional pain.”
After a period of confusion and stockouts, ARVs returned to the pharmacy at her health center. But other important services have not resumed.
“HIV testing in the community ended, and people who were newly diagnosed were left without counseling or support. Many did not know how to accept their status, how to take medicine correctly, or how to protect others. This has put many lives at risk,” says Mary.
“Stigma has increased a lot. Before the funding cuts, people living with HIV were served in special ART [antiretroviral treatment] clinics where there was privacy and understanding. After the cuts, HIV services were mixed with other chronic illnesses in one clinic. This change has caused fear, shame, and violence.”

“Community groups and volunteers have not been able to help enough. Most community programs stopped because of lack of funding.”
“Many people living with HIV are now alone and unsupported. Children and young people living with HIV are being forgotten.”
Mary would like to see a future when no children in her community are born with HIV. But without community services, she fears that more children are being born with HIV every month. Fortunately, there are already trained community members like herself with lived experience who are ready to continue their work to end the cycle.
“People living with HIV must be listened to, respected, and involved in decisions,” says Mary, noting that a woman struggling with an HIV diagnosis will have a more successful outcome if she has a friend who understands what she is going through and can provide advice and encouragement.
“Uganda needs to increase its own funding for HIV services and protect people living with HIV. If the government, donors, and partners work together, lives can be saved, and hope can be restored. HIV services must be safe, private, and close to the community.”
*Mary’s name has been changed to protect her privacy.

Mary, mentor mother from Uganda